Keep On Your Feet
The Foot, Ankle & Gait Clinic
Conditions We Treat

Accessory Bones
These can occur in various places in and around the foot and are very similar to the sesamoids under the big toe joint. The difference between the sesamoids and these little 'accessory bones' is that they are not required for function.
Occasionally they can be mistaken for fractures or bone growths. Their presence is not dramatically problematic but if they suddenly become painful after an injury, their removal may be worthwhile.

Achilles Tendinopathy
The Achilles tendon attaches the back of the heel to the calf muscles. There are three main calf muscles, and their role is to point the foot downwards.
The Achilles tendon is so significantly involved in the gait cycle that problems affecting it can be lifestyle-limiting.
Achiles tendon problems can be divided into different types:
1) Mid-portion
2) Insertional
3) Myotendinous junction
4) Intramuscular
It is important to make sure that you do have Achilles tendinopathy and that you don't actually have a plantaris tendinopathy - which would be pain on only the inside part of the tendon.

Ankle Sprain
Ankle sprains tend to affect the anterior talofibular ligament and the calcaneofiibular ligament. They can also damage the posterior talofibular ligatment and the tibiofibular ligament. Basically, there are lots of ways to 'traditionally' sprain an ankle on the outer side (pinky toe side) of the foot.
You can also sprain the ligaments on the inside of the ankle too, but this is much more difficult as these are incredibly strong and the structure of the ankle is protective.
There are a few considerations that are important when it comes to anke sprains, firstly, making sure that the injury is a sprain, and not a fracture.
Secondly, ensuring that you are rehabilitated so that you do not develop any long term issues or ankle instability in the future.
Statistically, about 70% of people who sprain their ankle still have problems with instability or pain at 7 years, so the proper management of ankle sprains is essential.

Athlete's Foot (Tinea Pedis)
As is the case with fungal toenails, the athlete's foot that lives on our skin is actually essential to ensuring that our skin stays healthy. We require all of the good and bad organisms to maintain an even number, otherwise the one organism may then start attacking the skin.
Although it is thought to be contagious, it is more likely that it is the result of our general health or the environment that we keep our feet in that might cause the development of foot fungus.
Podiatrists can help you to diagnose the foot fungus and advise the most appropriate treatment protocol for the fungus.
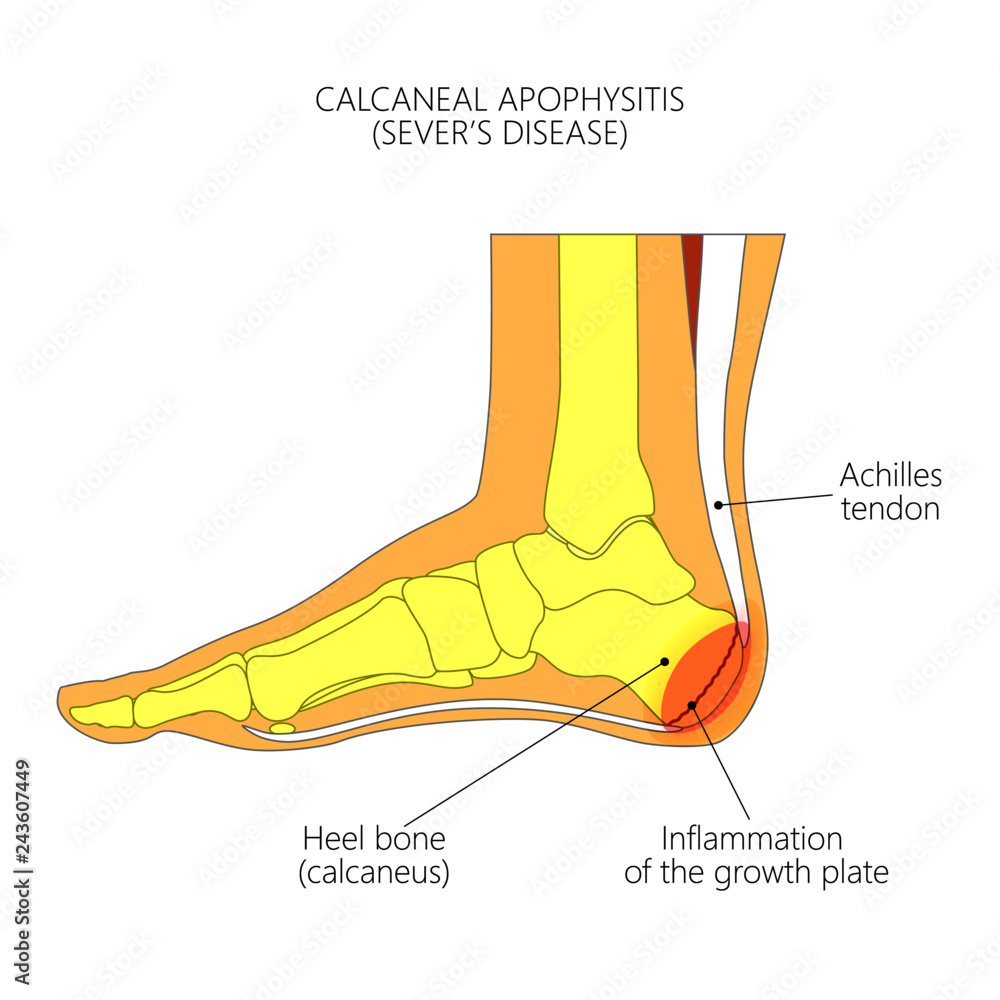
Calcaneal Apophysitis
It can be extremely painful for kids who have this and it can often cause a lot of concern for parents.
Let me start by reassuring you this is probably the most common cause of foot pain that I see in the under-16s.
When we are growing, the bones grow from regions called growth plates. These regions become 'active' during growth spurts, and are more suscepitble to irritation. As a result, sporty and active children will continue running around on this easily irritated structure and it can cause them severe pain.
There is no good reason to stop doing sports, but a careful balance of monitoring activity levels is important.

Calcaneal Oedema
Calcaneal' refers to the heel bone (properly called the 'calcaneus' or 'calcaneum'. 'Oedema' just means 'swelling'.
Calcaneal oedema very commonly occurs with plantar fasciiitis but is really more similar to calcaneal apophysitis - but the adult version! Let me reassure you, if you have finished growing, you will not be able to get calcaneal apophysitis.
Calcaneal oedema is simply bruising and can be really quite brutal to put up with. Unlike plantar fasciitis, it gets worse as time goes on during the day, and will feel like you are walking on a stone.
If you find that you get pain when you first get up and then have pain at the end of the day or if you have been walking around barefoot for a while, then it is quite likely you have calcaneal oedema. Likewise, if you are feeling pain in your foot when you are lying in bed or sitting on the sofa after a busy day, this is a more likely diagnosis.
Very rarely (I've not seen one yet, neither have my mentors who have hundreds of years of experience between them!), symptoms when you are off your feet can be associated with more sinister problems. This said, it is far more likely to be a back problem presenting in your feet.
Experienced podiatrists who diagnose and treat heel pain regularly will be able to clinically diagnose (hear your history, ask relevant questions and physically assess you) and differentiate between bruising, fractures, back problems causing heel pain and the big, bad stuff. Likewise, experienced podiatrists should be qualified to organise imaging to confirm your symptoms.

Capsulitis
Capsulitis is a very common issue and can occur for a variety of reasons, such as: stiff big toe joints, bunions, stubbing your toe, dropped metatarsals, rheumatoid and psoriatic arthritis and for a whole host of other reasons.
The presence of pain in a knuckle can be really quite debilitating and, if you have developed capsulitis: it is usually quite inconvenient as it generally occurs when people are trying to get fitter, healthier, or training for an event.
The number of treatments available to people with capsulitis is vast but diagnosis is essentail. First, it is incredibly improtant to make sure that you do not have a plantar plate injury (toe joint sprain) as this will be progressive unless managed properly.
Seeing a health professional who can organise diagnostic imaging would be your best bet to make sure that you get an accurate diagnosis. This being said, it is possible to get accurately diagnosed with just clinical assessment, but you are relying on the health professional knowing how good they are at diagnosing this condition.

Corns
Corns are particularly painful given t+F43hat they are 'just' hard skin. There are a variety of ways to treat corns and to prevent them recurring.
If you have a corn that is very painful and keeps coming back quickly then you might wish to consider an appointment to see if it can be prevented from coming back, or at least made to not return as quickly.
Often corns which are seasonal are the result of your preferred seasonal footwear. If the corn keeps on returning or is only painful in one or two pairs of shoes, then you might need to reconsider the shoes you wear.
To find out what the reason is for the corn or to find out whether or not I can prevent it coming back so quickly, feel free to get in touch.
The biomechanics of skin and feet are something that not many take an interest in, so I actually have a lot of practice and success in this area of podiatry.

Enthesitis
Enthesitis, otherwise known as enthesiopathy is where supporting structures attach onto a bone.
There are loads of entheses in the body, but the ones that are most often effected in the foot are the Achilles tendon, plantar fascia,tibialis posterior, peroneus brevis and tibialis anterior.
When you have enthesitis as a result of doing too much, then supports, exercises, anti-inflammatories, activity pacing and other strategies can be very effective and can quickly settle your symptoms.
If your symptoms are seemingly without a mechanical cause (idiopathic), then a more detailed history may be needed. Sometimes these conditions are the result of other problems you might have, such as psoriasis / IBS, some types of back pain, medicines you have taken or infections you have had recently.

Flat Feet
Flat feet are the result of either how you developed growing up or may be the result of injury or disease.
Having flat feet on their own does not mean that you have a specific problem, so, please do not worry about having them. Equally, having flat feet may pre-dispose you to certain musculoskeletal injuries BUT it will also potentially prevent you getting other injuries.
Being screened for flat feet and assessed as to whether you might need insoles or orthotics is helpful, but I would not necessarily go straight to having orthotics just because your arch profile is lower.
Flexor Tendinopathy
It is very unusual to develop flexor tendinopathy in the lesser toe flexors, but it is not as uncommon to develop this tendinopathy within the big toe flexor(s).
The complicating factor is that the big toe flexors run along the length of one of the bands of the plantar fascia, and so misdiagnosis of flexor tendinopathy is very common.
Once again, the early diagnosis and targeted management of this problem will speed up resolution and mean that you do not have time to create compensations that cause aches and pains in other parts of your body.

Fungal Nails
It is not unusual for people to get a fungal nail infection at some point in their life. Typically, a fungus gets in when the nail gets damaged through bad cutting, and it is not unusual for the fungus to be a part of the patients own 'special brew'.
We all have a variety of organisms on our skin, and we rely on them to keep our skin healthy. It is only when one organism gets an advantage over the others that an infection 'takes hold'.
The nail is often thought to be dead, but fortunately it was never alive - otherwise cutting it would hurt.
Note, if your parents or partner ever cut your nails and it hurt: this is not because they were cutting live nail, it's because they were cutting the live skin next to the nail!
It is very easy to manage an infection in the nail at the tip of the toe, and much hard to manage it when the infection is further back.
Getting to the nail sooner is preferable, but if you have left it, don't worry, I'm sure I'll still be able to help - one way or another!
Haemosiderosis
When you have poor upwards circulation, some blood may leak out of your veins and will take the red blood cells with it. This then means that any red blood cells that remain are broken down. Unfortunatley, the iron within the red blood cells does not get broken down and this stays in situ... hence, you've gone rusty

Hallux Rigidus
If you have noticed that your big toe joint is stiff or painful when walking, then it is possible you might have an arthritic.
You might have noticed some hard lumps have formed around the joint or that it seems like you have a bunion, but your toe still points straight forward.
It can be caused by injuries to the joint such as fractures or dropping something heavy on it, but it can also be the result of an active lifestyle (playing a lot of football or running), or you might just be a bit unlucky and have developed it because of how your foot functions.
A lack of movement, on it's own, does not necessarily require treatment. This being said, if it is causing concern then I might be able to reassure you, make some suggestions as to how to improve your symptoms or to discuss what the short, medium and long term complications might be for you.

Hallux Valgus, Hallux Abducto Valgus & Bunions
Hallux valgus is a condition that is often congenital (a genetic gift from our parents), however may become more severe with time.
If not causing any pain or discomfort, a hallux valgus does not require treatment. This being said, it can cause some biomechanical changes which will cause pain in other structures both in the foot and ankle as well as further up the body. Not everytime, but in some cases, that is.
The management will depend on the nature of your symptoms; some symptoms may require advice on lifestyle and changes to footwear. Other management strategies might include padding strategies, taping, foot exercises, orthotics, steroid injections, routine chiropody and possibly a referral for surgery.
Please note, it is incredibly difficult (for all intents and purposes: impossible) to 'reverse' a bunion without having surgery. The use of night splints has been found to be helpful in children under the age of ~14, but otherwise benefits are limited.
Hard skin / Callus / Hyperkeratosis
Callus forms on areas of high pressure and friction. It is not a bad thing to have, as it demonstrates that you have good circulation and that you are active.
Managing your callus is something that, as a podiatrist, I can help you with, but likewise I can teach you how best to manage your own callus.

Heel Pain
Heel pain is often diagnosed as plantar fasciitis, however, I see a lot of patients who think that they have this condition BUT their pain is not in their heel.
Although they do all the right things for heel pain, they are not necessarily doing anything useful for the symptoms that they have.
To treat something as heel pain - only manage it as a heel pain if your pain is under the heel, feels like you are walking on a stone OR you feel like you are being stabbed in the bottom of the foot.
Pain at the back of the heel must be managed differently to pain at the bottom of the heel.
Pain on the inside (big-toe side) of the ankle should also be managed differently to pain on the outside (pinkie toe side) of the ankle / heel bone.
Heel Spurs
Heel spurs occur as a result of a period of increased traction having occurred. This is often the result of having been overweight (currently or historically), but can also just be the result of repetitive 'overload'.
Heel spurs are better positioned as a description than a diagnosis. The reason that a heel spur being given as a diagnosis is unhelpful is because:
Heel spurs are lumps of bone that have grown as a way of the body responding to the extra traction going through the bone the structure joins to. Although pain fluctuates, the heel spur's size and position does not fluctuate... so if you have pain in one part of the heel and then a different part or you have a day without pain, that does not mean that the heel spur has gone.
Also, so many people have heel spurs and have no pain at all... so take it from me, you don't need to worry about that heel spur you were diagnosed with!

Ilio-tibial Band Syndrome (ITB)
The Iliotibial band is a structure that is important for posture and stability.
Many runners, particularly those who have flatter feet, will fall victim to iliotibial band issues. It is associated with pelvic drop and a high Q-angle, and thus learning ways to manage these can be very helpful.
The first thing is to make sure that the diagnosis is correct, and not a lateral knee compression or lateral collateral ligament strain, and once this has been checked, gait retraining with strengthening exercises can begin.

Ingrowing Toenails
Ingrowing toenails, contrary to popular belief, do not grow sideways. They also do not grow diagonally. The reason that a nail will ingrow is because there is either too much width of the nail compared to the amount of space available, the nail has been cut back too far and a sharp edge has been left, or the nail is very curved and sits under the level of the skin.
If you have a single episode of an ingrowing toenail that is only very slight, then you may be able to get away with just having the edge trimmed out.
This being said, a lot of ingrowing toenails tend to be a repetitive issue and will only continue to return. In these circumstances, it is possible to have the nail edge removed with a local anaesthetic to freeze the toe, and after this we can use a chemical on that part of the nail to make sure that it does not grow back.
If you attend and I suggest this, it is likely that I think this will continue to be an issue, and so I would say that you should definitely ask me why I think it would be, so that you can better understand your options.
Interdigital Bursitis
A bursa is a fluid filled structure - kind of like an airbag, that the body produces to provide a cushion to nearby structures.
Diagnosis, and differentiating it from a neuroma (swollen nerve) is quite hard to achieve without imaging, however is also not necessary.
The treatments for each problem are almost entirely the same, unless you are having surgery.
Although symptoms and problems in this region can be exceptionally painful for what they arae, I would recommend not rushing to surgery as the symptoms can be very easily managed with targeted treatment. Likewise, surgery is something which can both improve and worsen symptoms, so should really be used as a last resort in the event of symptoms being unrelenting despite good adherance to treatment plans.

Medial Tibial Stress Syndrome
(MTSS)
Tibial stress fractures can be exquisitely painful, but are typically only painful whilst running and sprinting, unless doing longer distances when even a jog may be problematic.
This is a particularly common problem in military recruits and those who take on a new training regime. Likewise, athletes who develop this in the middle of a training regime who ramp up their activity a bit too rapidly can struggle with this.
Pain is normally very localised to one particular spot on the back-side of the tibia on the inside of the leg,, but may also be generally tender in a region approximately 6-10cm in length.
Managed with a mixture of orthotics, footwear, strengthening and managing your activity levels. Other strategies for the treatment of Medial Tibial Stress Syndrome exist, but are not usually necessary. Sometimes including other specialists may also be necessary.

Metatarsalgia
Metatarsalgia literally means 'pain in the forefoot': 'metatars-' refers to the bones in the forefoot called metatarsals; 'algia' means 'pain' - just like 'analgesia' are painkillers (an = non, alge = pain, -esia = condition).
The number of causes of forefoot pain is vast and there are at least 20 common causes of forefoot pain... and three to four times that many that are less common.
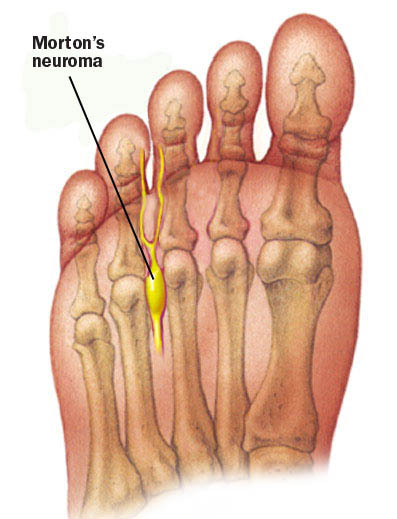
Morton's Neuroma
Neuroma' is technically misnamed since a neuroma between the metatarsal heads is actually a swelling of the nerve sheath, rather than a swelling of the nerve.
For a nerve to be a Morton's Neuroma, it should actually be causing discomfort in the space between the third and fourth metatarsal heads or into the third and fourth toes.
It can be difficult to differentiate a neuroma from intermetatarsal bursitis, and the principle emphasis in diagnosis should be based on history and clinical examination.
Treatments for neuroma pain typically focus on reducing the irritating factors and once you can get on top of these factors, your symptoms should mostly reduce or entirely resolve.
The biggest barrier to treatment is a desire to wear certain types of footwear. It is possible to work back into certain types of footwear that you will want to wear, but initially there will need to be some give and take! I'm always happy to negotiate, but keep in mind your neuroma is the terrorist that holds you hostage - I'm just trying to get the two of you into a happy place!

Osteoarthritis
This is the type of arthritis which is the result of thinning of the joint cartilage.
Although it is typically thought of as being the result of 'wear and tear' - like for people who did a lot of sports: the current science shows we should think of it as wear and repair. This basically means 'use it or lose it'. Although, somewhat obviously, there's a sweet spot to be reached.
No all arthritis is painful and in answer to the question "do I need surgery for arthritis" - the answer is a resounding 'no' (plus a "not necessarily...)

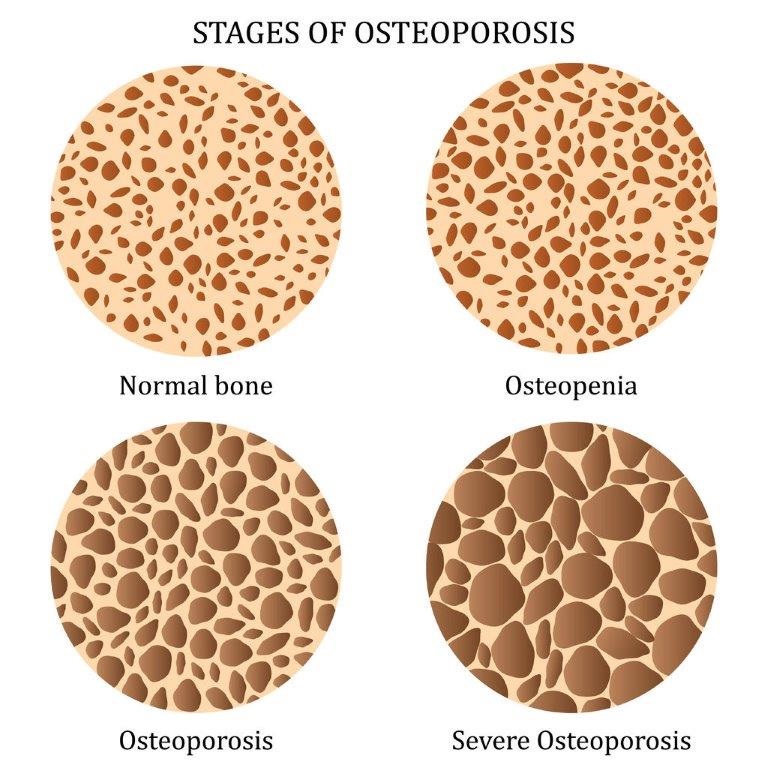
Osteoporosis
Literally meaning "porous bones", osteoporosis refers to a process described as de-mineralisaation.
Our body is constantly refreshing itself and renewing its structure, and bones are no different.
The bones in the body get broken down and new bone gets laid down regularly. In osteoporosis, the body breaks down bone faster than it can lay down fresh bone, and so the bone gets weaker.
To treat this, your GP might prescribe high strength suppliments, but you might also need to see a rheumatologist for medications that are more powerful.
Podiatry can assist in reducing strain through your joints and help to make you more comfortable.
Although it is typically associated with 'older people', it can also be associated with athletes who exercise 'too much' and also for girls / women with irregular periods. I will always screen for this, if your symptoms may be associated with osteoporosis.

Paranychia
Paranychia can be extremely painful and I see it quite often in people who have just had a manicure or pedicure (DIY or in a nail salon). The presence of an paranychia should be explored as, if it is associated with some local event such as cutting the affected digit or having had your nails cut and then become painful, it is quite likely there is an infection.
Although an infection is not a good thing to have, it is not necessarily something panic about. Good hygiene routines such as salt water bathing, application of anti-bacterial treatments, use of sterile dressings and sometimes releasing any infected pus can be highly beneficial.
Other times, it might be that a small edge of nail or hard skin needs to be removed to allow the soft tissue to stop being irritated.
As an HCPC registered podiatrist, I can issue a selection of antibioitcs for you at your appointment, and I can also write to your GP if you need an antibioitc that I cannot issue.

Patello-femoral Pain Syndrome
Previously known as chondromalacia patella (meaning 'bad cartilage of the knee cap'), this is an extremely common issue for athletes. It can also affect the less active population as well, particularly if they have some hypermobility or a flatter foot posture.
The pain you have is of the back of the knee cap being inflamed and then rubbing against the thigh bone. As the joint is immobile for a while, it can stiffen up, so you get 'cinema sign' (discomfort when sitting with the knee bent for a long time), and you might also get pain when going into a squat.
These symptoms can describe so many aspects of knee pain however, so the rule is: history first, then assessment.
The mainstay of treatment should always be rehabilitation which I can help with, but managing your biomechanics with running-gait retraining and using insoles can be excellent for keeping you doing what you love.
The best evidence says that one does not need custom insoles for PFPS, and this is correct in the majority of cases, HOWEVER, some feet do require more support to ease symptoms, and as a result, may need an insole that is semi-custom or even completely besopke.

Pitting Oedema
This can be caused by poor circulation, fluid retention, pregnancy, certain medications, steroids and diseases of the heart, liver or kidneys.
Minor pitting oedema can be resolved simply by putting your feet up. More severe cases of pitting oedema may require diuretics to help your body release the fluid, and may even require compression stockings to improve circulation.

Plantar Fasciitis
Contrary to popular belief, not all heel pain is plantar fasciitis. The plantar fascia is a very specific structure in the foot and is made up of three parts: the medial, central and lateral bands.
The pain typically occurs first thing in the morning on your first steps when you get out of bed; after extended periods of walking and when getting up from having been sat down.
The pain can only be under / on the very bottom-side of the heel AND/OR within the arch. Pain elsewhere in the heel foot, including on the back of the heel, is unlikely to be plantar fasciitis, and treating htis pain the same way as you would treat plantar fasciitis may make your pain worse.

Psoriatic Arthritis
An autoimmune condition common in those with psoriasis or IBS-like conditions.
Causes swelling in a small joints and will normally only affect one joint.
Podiatric management with insoles, footwear advice, injections, anti-inflammatory regimens will initially help however, you should be referred to a rheumatologist and/or dermatologist for optimum management and I can assist in facilitating this.

Rheumatoid Arthritis
An autoimmune condition common that primarily attacks the joints in the hands and feet. It can affect a number of other systems in the body too
Symptoms in the earliest stages will normally affect the little toe joint on both feet at the same time.
Podiatric management with insoles, footwear advice, injections, anti-inflammatory regimens will initially help however, you should be referred to a rheumatologist for optimum management and I can assist in facilitating this.
This condition used to cause severe deformities, however modern medications can almost entirely prevent the deterioration of joints with this condition now.
Sesamoiditis
Sesamoiditis is effectively a bruising of the small bones under the big toe joint.
It might feel like you are walking on a stone, you might notice bruising and will get worse the longer you are walking / running.
It is allso very common in dancers as well as rugby / football players. It can be quite debilitating, but is very easily managed with semi-bespoke insoles as well as a variety of treatment regimes.
Physiotherapy can be helpful, however I would strongly recommend that you also see a podiatrist. The services offered by physiotherapy will assist in the management, but insoles are necessary to get on top of the initial pain you have.

Shin Splints
The two most common diagnoses associated with shin splints are medial tibial stress syndrome and anterior compartment syndrome. Please see the sections for these for more details. To further read about my dislike of the term 'shin splints', please read on:
Shin splints has no meaning at all other than something to do with shins. I have heard the term shin splints used to describe pain in the 'shin' / ankle / front & back of the shins as well as the inside and outside of the shins. I have also had it suggested to me that I prescribe shin splints.
The number of causes of shin pain is vast and there are so many that it is not possible to list them within this post.

Sinus Tarsi Syndrome
Sinus tarsi syndrome occurs when there is too much movement in the joint or a lot of compression occurring.
This region is typically just a 'space', however, if you have had an injury that results in increased instability in the ankle; then you might develop synovitis or have scar tissue form within the joint.
Synovitis is a diagnosis for synovium (lubricating stuff) that has become inflamed within the ankle. This, combined with scar tissue formed within the joint as a result of the increased movement / injuries willthen become inflamed.
The inflammation then gets gradually worse as time goes on as the instability remains and with inflammation comes pain.
Diagnosis is the first thing that needs to happen. Once you have a diagnosis, the treatment can be targeted to your needs: managing the instability or managing the compression occurring.
Stress Fractures
The term 'fracture' covers a vast array of pathologies from slight irritation of the surface of a bone through to a bone being dust after you jump out of a plane.
Stress fractures effectively mean that there is a small crack in the outer part of the bone, but the structural integrity remains good unless you do not pay heed to your symptoms and continue to exercise through the pain you are experiencing, in which case you might find that you do end up converting a stress fracture to a true fracture.

Subungual Exostosis
A subungual exostosis is typically the result of an injury to the toe - this might be stubbing your toe, dropping something on it or someone demonstrating a lack of love for you with their heel.
As the nail grows forward over the bone in your toe, the nail has to either grow straight into the skin or up and over. This can cause the nail to either grow in a very rounded shape - turning it into a pincer nail, or can cause it to have a large growth coming out from under the nail.
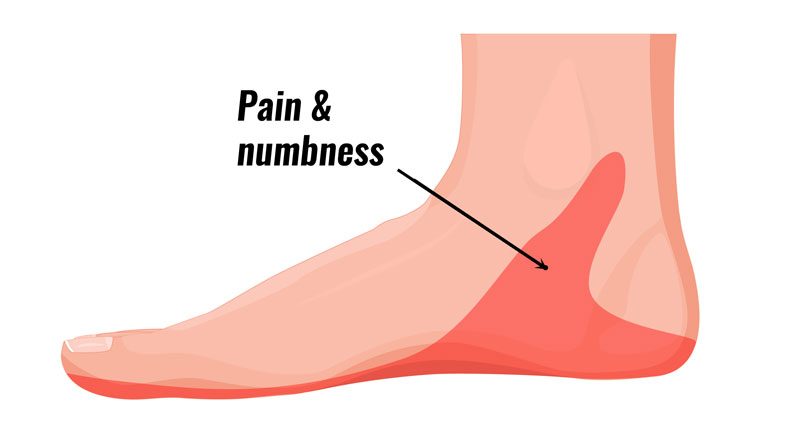
Tarsal Tunnel Syndrome
The tarsal tunnel is a space which the tibial nerve passes through to go into the bottom of the foot. Other structures also pass through this space including the tibialis posterior tendon, flexor hallucis longus and flexor digitorum longus.
If any of these structures become inflamed, or the soft tissues around it become inflamed, then you may develop burning, numbness or tingling symptoms in the forefoot or heel.
This can also be confused with problems occurring in your spine, so always make sure that you practitioner has checked for this.

Tenosynovitis
Tenosynovitis is the earliest stage of a tendon problem.
It can be excessively painful for what it is, but because it is the earliest stage of a tendon problem, it is also easy to manage if gotten on top of quickly.
There are a variety of ways to manage this problem including supports with tape, orthoses, supports, anti-inflammatories, exercises, draining the fluid and injections.
You do not typically need any imaging to confirm this, but it can be helpful. This condition can often be quite easily daignosed with nothing more than a detailed history.

Tibialis Posterior Tendon Dysfunction
Also known as Tibialis posterior dysfunction, posterior tibial tendon dysfunction or adult acquired flatfoot: this condition is associated with a lower arch, pronated foot type and is something which must be managed quickly when it occurs.
Split into multiple stages, this condition, if not managed quickly, is progressive and will cause deformity. It is the only common foot problem in an otherwise healthy population that should be managed quickly and agressively, with strong orthotics, exercises and close monitoring.
The tibialis posterior tendon attaches onto a bone caled the navicular and this bone is responsible for holding the arch up. If you start to feel pain on the inside of the ankle which is either painful when getting up from rest or on increased periods of walking, then you should get some assistance quickly.*
Please note, this is the only condition that I am stressing seeking help from someone specialised. Other conditions can be 'watchfully neglected'!
You will likely need a pair of insoles, to purchase some good quality trainers, potentially to lose weight and also to do exercises. Please do not hold off on booking until you have done these things - the number of people who delay getting assistance until they have tried the above end up requiring more treatment due to greater severity of the condition. It will save you money!

Toe Deformities
Toe deformities can occur for a huge number of reasons. You might have sprained the joint, broken the toe, had less-than-optimal foot mechanics or just have one the genetic lottery that resulted in your toes being misshapen.
Like with other 'deformities', the shape is not as important as the impact that the shape has on your daily life. If it has no impact and you just want treatment because it's there, I would say there are far better ways to spend time off your feet - in the Caribean drinking margaritas for a start...
If the joints within the toe are hurting or the toe is rubbing then you may benefit from treatment. This may range from strategies like taping and bracing, right through to considering surgical intervention.
As a general rule, I normally suggest seeing a podiatrist who is excellent at identifying the cause and can then guide you on the surgical and non-surgical management of these problems. Some surgeons will be aware of the alternative options whilst others will be very keen to perform surgery. Neither is 'right' or 'wrong', but I think a balanced discussion is necessary to ensure optimum outcomes.

Verruca
Verrucae are caused the the Human Papilloma Virus and, in the case of those that occur on the feet, they are not the types of virus that can turn malignant.
Verrucae are most easily mixed up with callus and corns, and may also co-exist with callus and corns.
Their treatment relies on stimulating the body to identify and attack the virus. Unfortunately there are no medications that actually kill the virus when used on humans.
To stimulate the immune system, we have to cause damage to skin under and around the verruca to bring white blood cells to the area so that the body can attack the lesion. Verrucae have many mechanisms that also make them very hard to treat, but the first thing to do is to work out whether it is a verruca or a corn!
The black dots are not the virus, they are just bits of blood that has leaked into the lesion as the hard skin builds up.